Bone Densitometer (DEXA Scanner): understand the pranciples behind this machine
Table of Contents
- Introduction — why DEXA still matters
- What is a Bone Densitometer (DEXA)? — definition and core uses
- A short history of bone densitometry
- How DEXA works — the physics and imaging principle
- Types of DEXA hardware — pencil-beam, fan-beam, and array detectors
- Key performance metrics and clinical outputs (T-score, Z-score, BMD, precision)
- Standard clinical protocols and scan sites (spine, hip, forearm, whole-body)
- Advanced applications: vertebral fracture assessment, body composition, pediatric use
- DEXA vs other bone assessment technologies (QCT, HR-pQCT, ultrasound)
- Safety and radiation dose — risks and minimization
- Maintenance, quality control, and acceptance testing (for biomedical engineers)
- Procurement, cost, and accessibility considerations
- Future trends: AI, TBS, higher resolution, and theranostics interplay
- Simple analogies to clarify concepts
- Final summary — key takeaways
- References
1. Introduction — why DEXA still matters
Osteoporosis is a silent, high-impact public-health problem: low bone density increases fracture risk, morbidity and healthcare costs. Dual-energy X-ray absorptiometry (DEXA or DXA) remains the clinical gold standard for measuring bone mineral density (BMD), diagnosing osteoporosis, monitoring therapy, and estimating fracture risk. Its combination of accuracy, very low radiation dose, speed and standardized outputs (T-score/Z-score) makes it central to patient care, research, and population screening strategies.
Keywords: DEXA, Bone Densitometer, bone mineral density, osteoporosis, DXA scanner
2. What is a Bone Densitometer (DEXA)?
A Bone Densitometer (DEXA scanner) is a specialized low-dose X-ray system designed to quantify the mineral content of bone. Unlike diagnostic radiographs that show structure, DEXA provides quantitative measurements (g/cm²) that are converted into T-scores and Z-scores for clinical interpretation. DEXA systems also frequently include software for body composition (fat and lean mass) and vertebral fracture assessment (VFA).

Primary clinical uses:
- Diagnose osteoporosis/osteopenia (WHO criteria)
- Predict fracture risk (often combined with FRAX)
- Monitor BMD changes during therapy
- Body composition analysis (research, sports medicine)
3. A short history of bone densitometry
Bone densitometry evolved from single-energy techniques in the 1960s to dual-energy X-ray absorptiometry in the 1980s, which improved accuracy and reduced soft-tissue confounding. Commercial DEXA systems from major vendors (e.g., Hologic, GE Lunar) standardized clinical practice in the 1990s. Over subsequent decades, software improvements, whole-body analysis, and secondary metrics (trabecular bone score, fracture risk tools) expanded DEXA’s role.
4. How DEXA works — the physics and imaging principle
DEXA uses two X-ray energy levels to separate bone from soft tissue:
- The system emits two X-ray beams (low and high effective energy).
- Bone and soft tissue attenuate (absorb) the beams differently.
- By measuring attenuation at both energies, the algorithm mathematically removes soft-tissue contribution and computes bone mineral content (BMC) and bone area, yielding BMD = BMC / area (g/cm²).
This dual-energy approach reduces soft-tissue artifacts that would confound single-energy measurements. Modern DEXA uses fan-beam or array detectors with rapid acquisition and digital processing.
5. Types of DEXA hardware — pencil-beam, fan-beam, and array detectors
- Pencil-beam DEXA (older): a narrow collimated beam scans across patient; robust and simple but relatively slow.
- Fan-beam DEXA (modern): wider beam and linear detector arrays allow faster scans and higher spatial resolution; requires careful geometric calibration and can show magnification artifacts if not aligned.
- Array detectors / digital systems: improve speed, image quality and enable whole-body composition analysis.
Choice affects scan time, resolution, potential artifacts and throughput.
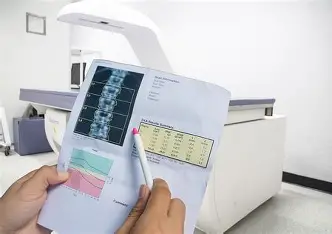
6. Key performance metrics and clinical outputs
- BMD (g/cm²): primary quantitative output.
- T-score: number of standard deviations (SD) the patient’s BMD is from the young-adult mean — used for osteoporosis diagnosis (T-score ≤ −2.5 = osteoporosis).
- Z-score: SD from age- and sex-matched mean — used mainly in pediatrics and secondary osteoporosis assessment.
- Precision (repeatability): typically measured as coefficient of variation (CV%) from repeated scans; precision is essential for determining the least significant change (LSC) to decide if therapy response is real. Typical LSC for spine/hip is on the order of 3–5% depending on device and operator.
- FRAX: fracture risk calculator can incorporate femoral neck BMD for 10-year fracture probability.
- Trabecular Bone Score (TBS): an index derived from lumbar spine DEXA images that provides information on trabecular microarchitecture (not a direct density measure).
7. Standard clinical protocols and scan sites
Recommended routine sites:
- Lumbar spine (L1–L4) — sensitive to early bone loss.
- Proximal femur (total hip, femoral neck) — important for fracture risk and monitoring.
- Distal radius (forearm) — alternative when spine/hip not available.
- Whole-body — used mainly for body composition, or research.
Scan protocols must adhere to ISCD (International Society for Clinical Densitometry) standard positioning and reporting guidelines to ensure comparability.
8. Advanced applications
- Vertebral Fracture Assessment (VFA): lateral spine images acquired on DEXA detect prevalent vertebral fractures with low dose.
- Body Composition: reliable whole-body fat and lean mass estimates for sarcopenia and metabolic research.
- Pediatric DEXA: uses Z-scores, size-adjusted outputs, and pediatric reference data; requires technician expertise.
- Serial monitoring: therapeutic monitoring requires consistent positioning and machine/operator precision to detect clinically meaningful BMD change.
9. DEXA vs other bone assessment technologies
- Quantitative CT (QCT): provides volumetric (mg/cm³) BMD and separate trabecular cortical analysis but at much higher radiation and cost. QCT is useful for spine when DEXA is confounded (e.g., severe osteophytes).
- HR-pQCT: research tool for microarchitectural assessment of peripheral sites (very high resolution, research only).
- Ultrasound (QUS): portable, radiation-free screening tool (heel), but less precise and not interchangeable with DEXA.
Bottom line: DEXA remains the clinical standard for diagnosis, monitoring and widely used thresholds.
10. Safety and radiation dose
DEXA uses very low radiation — typical effective dose per standard spine/hip exam is about 0.001–0.005 mSv (fractions of a chest X-ray). Even repeated scans have minimal radiation risk. Operators must still follow ALARA principles: appropriate scan region, correct positioning and avoiding unnecessary repeats.
11. Maintenance, quality control, and acceptance testing (for biomedical engineers)
Quality assurance is critical for diagnostic confidence.
Daily/Weekly QC:
- Phantom scans: daily or weekly (manufacturer recommended) to track BMD value stability (mean and SD).
- Uniformity and noise checks: identify detector drift.
- Warm-up procedures for the X-ray tube.
Precision & acceptance testing (on installation):
- Phantom accuracy: compare measured to manufacturer reference values.
- Cross-calibration: if replacing a scanner, perform cross-calibration phantom scans to allow longitudinal continuity of patient data.
- Precision assessment: perform repeated scans on volunteers or phantoms to compute CV% and LSC.
Preventive maintenance:
- Mechanical (table travel, arm), electronic (detector), and software updates.
- Record keeping: log daily phantom results, service interventions, and performance trends.
Troubleshooting signals:
- Sudden drift in phantom mean → detector or calibration issue.
- Increased image noise → detector, grounding, or power problem.
12. Procurement, cost, and accessibility
Price ranges (indicative):
- Basic systems: ~$45,000–$70,000 USD
- Advanced whole-body systems with composition packages: $80,000–$130,000 USD
Total cost of ownership (TCO) includes:
- Installation, floor loading, local shielding (minimal), training, annual service contracts, phantom and calibration supplies, software licenses and potential cross-calibration costs.
Accessibility: portable and smaller units make DEXA accessible in community clinics and mobile screening units; reimbursement policies and screening guidelines drive utilization.
13. Future trends and innovations
- AI and automation: automated vertebral fracture detection, scan quality assessment, and improved precision estimation.
- Enhanced metrics: wider adoption of Trabecular Bone Score (TBS) and other texture analyses to complement BMD.
- Integration with risk models: seamless incorporation of DEXA outputs with FRAX and other clinical decision tools.
- Improved resolution & detectors: gradual hardware advances for better precision and lower dose.
- Portable high-precision DEXA and population screening: mobile units paired with telemedicine for outreach.
14. Simple analogies to demystify DEXA
- DEXA is a “precision scale for bones.” Instead of weighing the whole body, DEXA tells how much mineral is contained within a square centimeter of bone.
- Dual energy is like two colored lights shining through a curtain: comparing how red vs blue pass through tells you what the curtain is made of.
15. Final summary — key takeaways
- DEXA (Dual-Energy X-ray Absorptiometry) is the clinical gold standard for measuring bone mineral density and diagnosing osteoporosis.
- It produces quantitative outputs (BMD) and standardized scores (T-score/Z-score) used in clinical decision-making.
- DEXA is fast, safe (very low dose), and cost-effective, with broad applications including VFA and body composition.
- Biomedical engineers must implement robust daily QC, cross-calibration, and precision testing to ensure reliable longitudinal data.
- Future directions include AI, TBS and microarchitectural markers, and improved detector technologies.
16. References
- International Society for Clinical Densitometry (ISCD). Official Positions and Technical Review, latest edition.
- World Health Organization (WHO). Assessment of fracture risk and its application to screening for postmenopausal osteoporosis, WHO Technical Report Series.
- Blake GM, Fogelman I. The role of DXA in the diagnosis and treatment of osteoporosis. Bone, 2007.
- Njeh CF, Hans D, et al. Comparison of DEXA and QCT for assessing bone mineral density. Phys Med Biol, 2019.
- Baim S, Wilson CR. Reliable use of bone densitometry in clinical practice — manufacturer and regulatory guides.
- ISCD 2019 Adult and Pediatric Official Positions (for scanning protocols and reporting standards).
