Dental Imaging Systems: Technology, Principles, and Clinical Applications in Modern Dentistry
Table of Contents
- What Are Dental Imaging Systems
- A Short History of Dental Imaging
- How Dental Imaging Works: The Imaging Principles
- Key Hardware Components
- Clinical Applications & Use Cases
- Dental Imaging vs Other Radiology Modalities
- Safety & Radiation Dose: Risks and Minimization
- Maintenance & Technical Considerations (for Biomedical Engineers)
- Cost & Accessibility
- Future Innovations & Trends
- Simple Analogies to Demystify Dental Imaging
- Final Summary
- References
1. What Are Dental Imaging Systems
Dental Imaging Systems are medical devices that produce detailed images of teeth, jawbones, and surrounding oral structures.
They are fundamental tools in diagnosing oral diseases, planning surgeries, and monitoring dental treatment outcomes.
Modern dental imaging systems include several modalities:
- Intraoral X-rays (bitewing, periapical, occlusal)
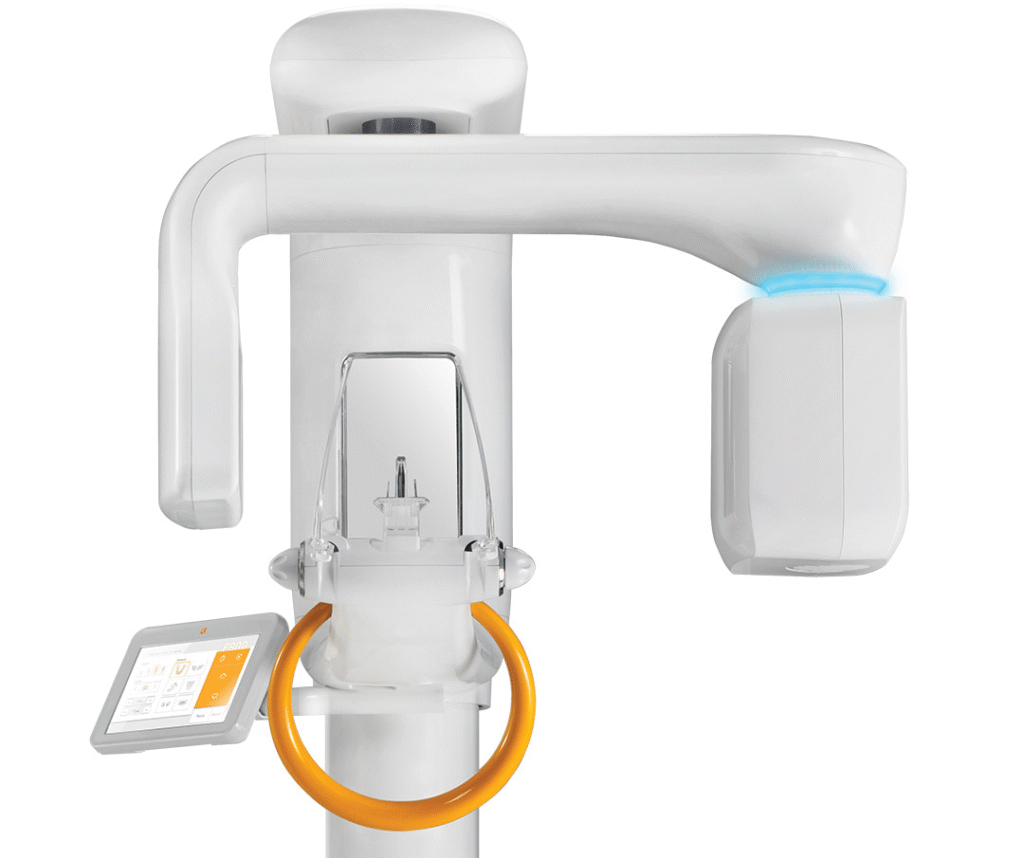
- Panoramic imaging (OPG)
- Cephalometric radiography
- Cone Beam Computed Tomography (CBCT)
- Intraoral digital sensors and cameras
Each system serves a unique diagnostic purpose — from routine cavity detection to complex 3D surgical planning.

2. A Short History of Dental Imaging
- 1895: Wilhelm Conrad Röntgen discovered X-rays — dental imaging began soon after.
- 1905: First dental X-ray unit was introduced.
- 1970s: Film-based panoramic imaging became standard in dental clinics.
- 1990s: Transition from analog to digital radiography (using CCD and CMOS sensors).
- 2000s–Present: 3D CBCT (Cone Beam CT) revolutionized dental and maxillofacial imaging — offering volumetric detail with low radiation.
Today, digital dental imaging is essential for precision diagnostics, implant planning, orthodontics, and facial surgery.
3. How Dental Imaging Works: The Imaging Principles
All dental imaging systems are based on X-ray attenuation, where X-rays pass through tissues and are absorbed differently depending on tissue density.
- Hard tissues (like enamel and bone) absorb more X-rays → appear white.
- Soft tissues absorb less → appear gray.
- Air spaces absorb almost none → appear black.
In digital systems, the X-ray photons are detected by sensors (CCD/CMOS or flat-panel detectors), converted into electrical signals, and processed into high-resolution digital images.
Simple Analogy:
Think of X-rays as a flashlight shining through a translucent object.
Where the object is thicker (like bone), less light passes through — the detector records that “shadow” to reconstruct an image of internal structures.
4. Key Hardware Components
| Component | Function |
|---|---|
| X-ray Tube | Produces controlled X-ray beam for imaging. |
| High-Frequency Generator | Regulates voltage (kVp) and current (mA). |
| Collimator | Shapes and narrows the X-ray beam to the target region. |
| Detector / Sensor | Captures X-rays (CCD, CMOS, PSP plates, or flat-panel). |
| Control Console & Software | Manages exposure settings, image capture, and processing. |
| Patient Positioning System | Ensures reproducible and stable image geometry. |
5. Clinical Applications & Use Cases
- Caries (cavity) detection
- Endodontic (root canal) evaluation
- Implant planning using 3D CBCT
- Orthodontic and cephalometric analysis
- Detection of cysts, tumors, and jaw pathologies
- Trauma and fracture assessment
- Sinus and TMJ (temporomandibular joint) evaluation
6. Dental Imaging vs Other Radiology Modalities
| Modality | Main Use | Advantages | Limitations |
|---|---|---|---|
| Dental X-ray / OPG / CBCT | Teeth, jaw, oral cavity | High detail, low dose, 3D capability (CBCT) | Limited to head/neck region |
| CT Scan | Whole-body or craniofacial imaging | Wide coverage, soft-tissue detail | Higher radiation, costly |
| MRI | Soft tissue, nerves, joints | Excellent soft-tissue contrast | Poor for bone imaging |
| Ultrasound | Soft-tissue evaluation | Radiation-free | Limited use in dental hard tissues |
Thus, dental imaging remains the most specialized and efficient approach for oral diagnostics.
7. Safety & Radiation Dose: Risks and Minimization
Although dental imaging uses ionizing radiation, dose levels are extremely low compared to other modalities.
| Exam Type | Average Dose (mSv) |
|---|---|
| Intraoral X-ray | 0.005 |
| Panoramic (OPG) | 0.02 |
| Cephalometric | 0.01 |
| CBCT | 0.05–0.2 |
Radiation safety techniques include:
- Lead aprons and thyroid collars
- Collimation and filtration to reduce beam spread
- Automatic exposure control (AEC)
- Regular calibration and QA programs
In perspective — a full dental CBCT scan gives less radiation than a short commercial flight.
8. Maintenance & Technical Considerations (for Biomedical Engineers)
Biomedical engineers ensure the accuracy, safety, and uptime of dental imaging systems.
Routine maintenance checklist:
- X-ray tube output verification and calibration
- Detector uniformity and sensitivity checks
- Mechanical alignment of OPG/CBCT gantry
- Software updates and DICOM/PACS integration tests
- Radiation leakage and dose rate monitoring
Tip:
Detector calibration drift or misalignment often causes image artifacts — early QA detection prevents costly re-scans and downtime.
9. Cost & Accessibility
| System Type | Approximate Cost (USD) | Typical Setting |
|---|---|---|
| Intraoral Digital X-ray | $10,000–$25,000 | Private clinics |
| Panoramic (OPG) | $25,000–$40,000 | Dental centers |
| Cephalometric Combo Unit | $40,000–$60,000 | Orthodontic centers |
| CBCT 3D Scanner | $70,000–$150,000 | Hospitals & advanced dental facilities |
Maintenance is moderate — mainly software, detectors, and X-ray tube replacement every 4–6 years.
10. Future Innovations & Trends
- AI-Based Caries and Lesion Detection – automatic image interpretation.
- Low-Dose 3D CBCT Protocols – advanced dose-reduction algorithms.
- Hybrid OPG-CBCT Systems – offering 2D and 3D modes in one unit.
- Cloud-Connected Dental Imaging Platforms – for remote access and tele-dentistry.
- Augmented Reality Integration – 3D implant planning and surgical navigation.
The future of dental imaging is AI-driven, patient-centric, and cloud-integrated.
11. Simple Analogies to Demystify Dental Imaging
Imagine trying to look inside a solid pearl without breaking it.
Dental imaging systems act like a “safe flashlight” that reveals internal structures — tooth roots, nerves, and bone — all without touching or damaging them.
That’s how dentists diagnose hidden problems before pain even begins.
12. Final Summary
- Dental Imaging Systems are vital for modern diagnostics, implantology, and orthodontics.
- They rely on low-dose X-ray technology to visualize hard and soft tissues.
- CBCT scanners enable detailed 3D analysis of oral structures.
- Biomedical engineers maintain accuracy, calibration, and radiation safety.
- The field is moving toward AI, cloud integration, and ultra-low-dose imaging.
13. References
- American Dental Association (ADA). Guidelines for Dental Radiographic Examinations, 2023.
- European Commission. Radiation Protection No. 172: Cone Beam CT in Dental Radiology.
- Scarfe WC, Farman AG. What is Cone-Beam CT and How Does it Work? Dent Clin North Am, 2008.
- Hounsfield GN. Advances in Dental Radiography. Br J Radiol, 1995.
- IAEA. Radiation Protection in Dentistry and Oral Radiology: Safety Reports Series No. 104.
